In-Vitro Fertilization
In-vitro fertilization (IVF) is a method of fertility treatment in which the sperm and the egg (oocyte) are combined in a dish in the laboratory for fertilization to occur. Embryos develop in an incubator for several days. Your physician can transfer a resulting embryo to the uterus to develop naturally, while extra embryos are frozen and stored in the lab for future pregnancy attempts.
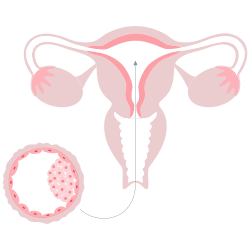
In a normal menstrual cycle, just one egg each month develops and matures. The egg matures within a fluid-filled structure on the ovary called a “follicle.” Once mature, the egg is released and travels down the Fallopian tube. Sperm travel from the vagina into the uterus and then up into the Fallopian tube, where fertilization occurs. The fertilized egg develops into an embryo. The growing embryo travels down the Fallopian tube into the uterus, where it implants approximately 5-6 days later.
IVF bypasses the Fallopian tubes, and accordingly, patients with damaged or absent Fallopian tubes can become pregnant. IVF is used to overcome endometriosis, male factor infertility, ovulatory dysfunction, advanced maternal age, and unexplained infertility.
Adore Fertility offers a variety of modifications to the standard IVF process to help patients with specific disorders and customize treatment plans. We provide intracytoplasmic sperm injection (ICSI) for couples with male factor infertility, preimplantation genetic testing for aneuploidy (PGT-A) for patients who want to screen their embryos for chromosomal abnormalities, preimplantation genetic testing for a monogenic disease (PGT-M) for couples with a single gene disorder, and assisted hatching of embryos for patients.
The IVF cycle includes five basic phases.
Step 1: Ovarian Stimulation
Step 2: Egg Retrieval
Step 3: Sperm Collection/Retrieval
Step 4: Fertilization & Embryo Development
Blastocysts can also be biopsied at Adore Fertility for preimplantation genetic testing (PGT) to determine if they are chromosomally normal. The biopsied cells are transported to a genetics lab for testing, while the blastocyst/s are frozen and stored at Adore Fertility. It takes approximately 2 weeks for the genetics lab to release the PGT report to your doctor. In a future FET cycle, a chromosomally normal embryo can be thawed and transferred to your uterus.
Step 5: Embryo Transfer (Fresh vs. Frozen)
Step 5 is the embryo transfer procedure. An embryo transfer can occur at the following times:
- On day 3 of your fresh cycle.
- On day 5 of your fresh cycle when the best-quality embryos have developed into blastocysts.
- On day 5 of a frozen embryo transfer cycle (FET). In a FET cycle, typically one blastocyst is thawed for transfer into the uterus to attempt pregnancy.
You will remain on hormones throughout the first trimester to support your uterine lining, called the endometrium.
Many fertility centers are moving to “Freeze All” cycles and FET cycles only. Some studies have suggested slightly higher pregnancy rates in the FET cycle. The reason why FET cycles may result in higher pregnancy rates is that during the FET cycle, the uterus is not exposed to the ovarian stimulation medications and supraphysiologic estrogen levels common in a fresh cycle. Thus, by freezing all good-quality embryos and allowing your body to recover, you can return for a FET cycle that allows a more natural environment for the transferred embryo to implant.
With a FET cycle, you do not undergo multiple injections of gonadotropins as you did during your fresh cycle. Instead, estrogens are prescribed to prepare your uterus. After 5-6 days of progesterone (injectable and/or vaginal), you then come in for your frozen embryo transfer procedure. Before your scheduled procedure, your embryo is thawed by an embryologist in the laboratory. Next, the embryologist loads your embryo into the tip of a soft, flexible catheter that is attached to a syringe. The loaded catheter is handed to your doctor, who slowly passes the tip of the catheter into your uterus through the cervix under ultrasound guidance. Then the embryo is carefully released into your uterus as your doctor gently presses the plunger. The embryo transfer procedure takes approximately 10 minutes, and no anesthesia is usually necessary.
Recent Articles
Choosing the Right Fertility Clinic: Questions to Ask Before You Decide
[dsm_blob_image blob_image="https://www.adorefertility.com/wp-content/uploads/2023/05/350377175_242668685060614_490906324096506677_n.jpeg" alt="fertility clinic" title_text="What-To-Do-While-You-Wait" blob_shapes="image_thirdteen" blob_position="bottom"...
Diet and Lifestyle Tips for Boosting Fertility
[dsm_blob_image blob_image="https://www.adorefertility.com/wp-content/uploads/2024/07/shutterstock_2390593521.jpg" alt="Diet and Fertility" _builder_version="4.26.0" _module_preset="default" global_colors_info="{}"...
Cutting-Edge Fertility Treatments: What’s New in 2024
[dsm_blob_image blob_image="https://www.adorefertility.com/wp-content/uploads/2024/07/shutterstock_2043915086.jpg" alt="Fertility Treatments in 2024" blob_shapes="image_two" image_height="350px" _builder_version="4.25.2" _module_preset="default"...
Top 10 Fertility Medications Recommended by Experts for Boosting Conception
[dsm_blob_image blob_image="https://www.adorefertility.com/wp-content/uploads/2024/05/shutterstock_2159141553.jpg" alt="Fertility Medications" blob_shapes="image_two" image_height="350px" _builder_version="4.25.1" _module_preset="default"...




